AAPI Mental Health
AAPI (Asian/American Pacific Islander) Mental Health has been an important focus within my practice. As someone who grew up in an Asian-American household, I recognize the unique challenges and barriers that Asian-Americans face when seeking out mental health treatment. I have also presented on this topic at the Los Angeles County Psychological Association (LACPA) as part of an initiative to help train other mental health providers.
The pan-ethnic term, Asian-American, originated in the 1960s and was expanded to include Pacific Islanders in the 1980s. AAPI are the fastest-growing racial/ethnic demographic in the country. In fact, the US Asian-American population is projected to reach 46 million by the year 2060. It is important to disaggregate the term AAPI given the vast heterogeneity of the group. The AAPI community consists of approximately 50 subpopulations coming from more than 20 countries. Native Hawaiians and Pacific Islanders are defined as persons having origins in any of the original peoples of Hawaii, Guam, Samoa, or other Pacific Islands. The AAPI community can experience very different socioeconomic outcomes. For example, the NHPI (Native Hawaiian/Pacific Islander) child poverty rate is more than double than that of Asian-American children.
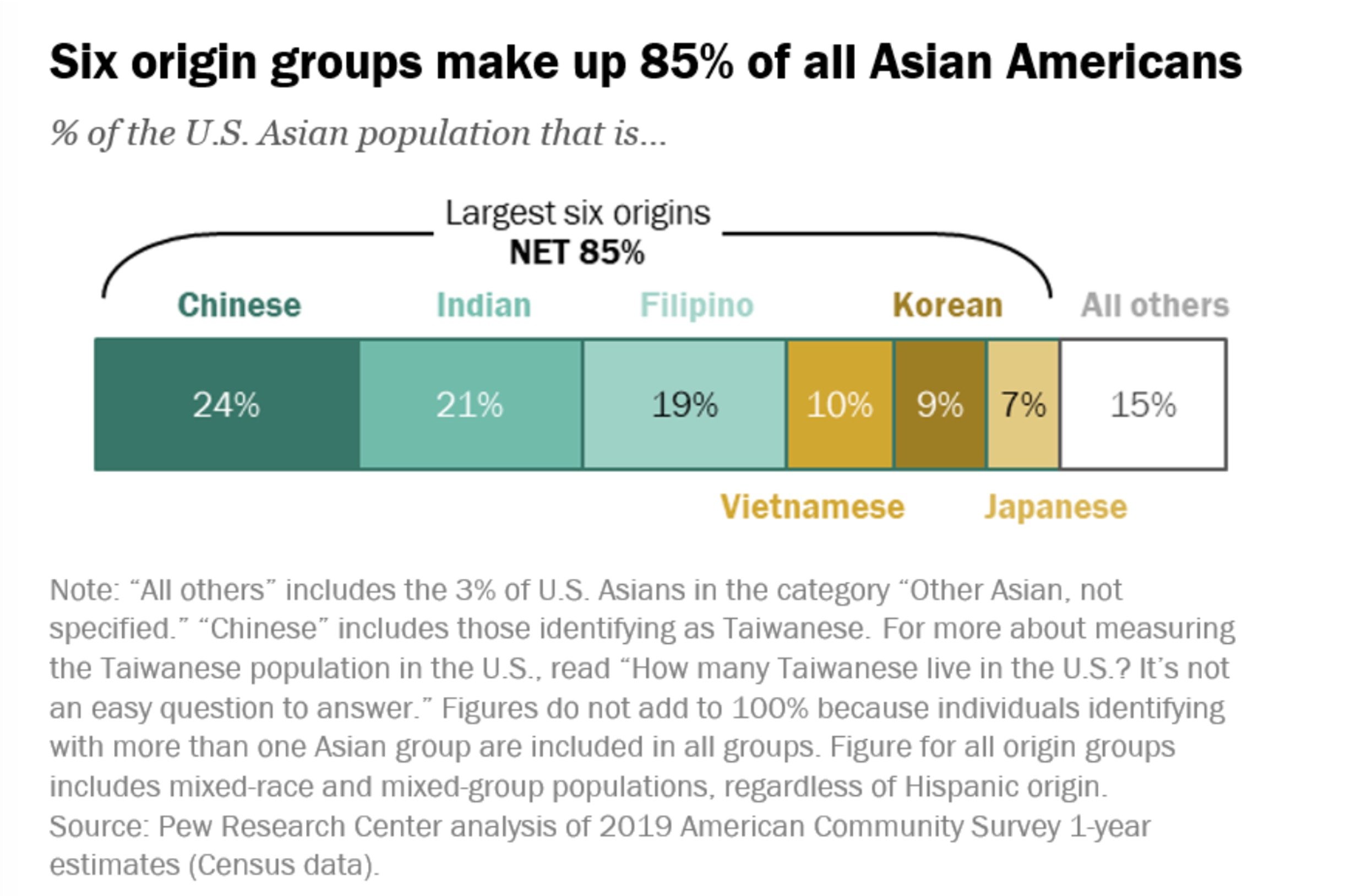
Within the US, around six origin groups make up 85% of all Asian-Americans:
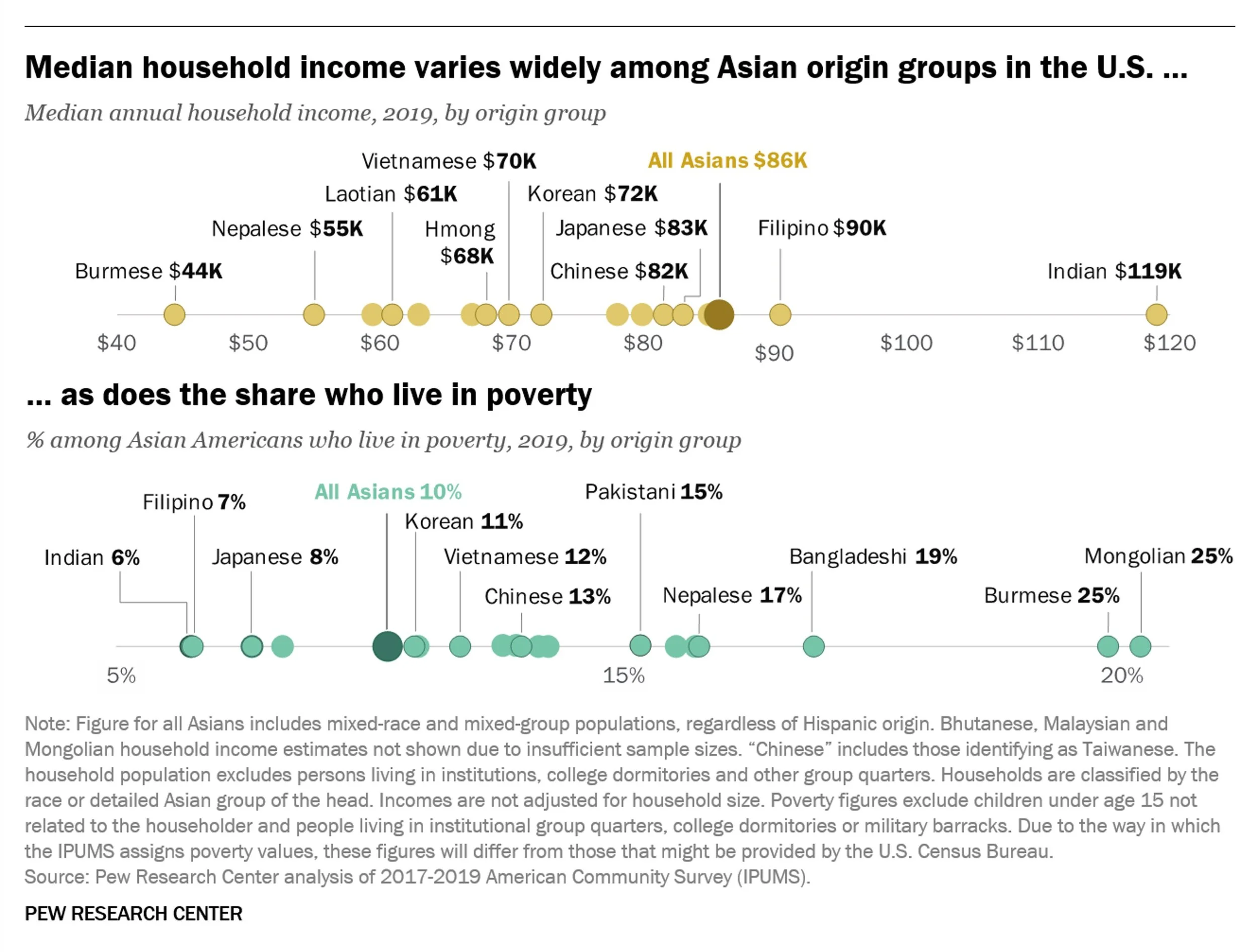
There is also significant variability in median household income:
As displayed on the graph, Indian-Americans and Filipino-Americans have the highest median income among Asian-American subgroups. Most of the other groups fall well below the national median for Asian Americans.
Mental Health Disparities
AAPI are the least likely to seek out mental health services compared other racial/ethnic groups in the US.
AAPI tend to underuse services unless they are culturally and linguistically compatible.
Based off of research, around 2.7 million AAPIs have a mental and/or substance use disorder.
https://www.psychiatry.org/psychiatrists/diversity/education/best-practice-highlights/working-with-asian-american-patients
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5615590/
Treatment Barriers
In order to understand how to move forward, it is important to get a full grasp of the current treatment barriers for AAPI:
Model Minority Myth
The perception that many AAPI experience of being expected to achieve a higher degree of socioeconomic success than the population average. This creates an unreasonable pressure to meet familial and societal expectations and can also lead to shame in seeking out support when struggling with mental health.
Stigma and Shame
A lack of understanding about mental health and associated stigma can lead to denial or neglect of mental health issues. At times, mental health can be viewed as a source of shame or burden within a community or family system.
Lack of Cultural Competency Amongst Providers
A lack of cultural competency amongst mental health provders can lead to the under-diagnosis and over-diagnosis of mental health problems amongst AAPI. For example, South Asians have been shown to present with more somatic experiences of anxiety. They can present in ways that do not meet the threshold level for certain mental health diagnostic criteria.
Immigration Status
Understandably, a fear of immigration status and associated concerns regarding deportation can limit seeking out care.
Lack of Involvement of AAPI Community Leaders and Family Members
It is important to have community and family support in encouraging individuals to seek out mental health treatment.
Intergenerational Trauma
Many AAPI navigate the experience of intergenerational trauma. Intergenerational trauma and historical trauma have been used interchangeably and reference the subjective experiencing and remembering of events in the mind of an individual or the life of a community that passed from adults to children in cyclic processes as “collective emotional and psychological injury.” Intergenerational trauma includes the impacts of individual experiences of trauma outside of the context of structural oppression.
Here is a chart listing out just some of the historical events connected to AAPI intergenerational trauma:
India-Pakistan Partition
US Colonization of the Philippines
US Nuclear Bombing of Hiroshima and Nagasaki
Chinese Civil War
Korean War
Vietnam War
Sri Lankan Civil War
Intergenerational trauma can present in may ways. It can look like:
Sense of shame and guilt to live up to the sacrifice of parents
Perfectionism and competitiveness
Anxiety about the future
Limiting shaping of identity
Making major life decisions with trauma in mind
Enmeshment/Co-dependency
Elevated suicide rate
Moving Forward
By better understanding the above, we can work towards creating a more tailored mental health experience for AAPI. Important interventions to keep in mind include:
Recognizing the impact of collectivism present in many AAPI communities on both supporting and serving as a barrier to mental health treatment.
Leveraging the positive power of community (involving community elders and religious leaders)
Inquiring about traditional beliefs (such as Yin/Yang concept of health/disease or the experience of mental health through somatic symptoms for some groups)
Incorporating traditional interventions (such as yoga, tai-chi, breathing exercises)
Being aware of the potential harm of underdiagnosis and misdiagnosis of Asian-American/Pacific Islander individuals.
Sources:
https://www.pewresearch.org/short-reads/2021/04/29/key-facts-about-asian-americans/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5615590/
https://www.psychiatry.org/psychiatrists/diversity/education/best-practice-highlights/working-with-asian-american-patients
https://journalofethics.ama-assn.org/article/historical-trauma-and-descendants-well-being/2021-06